The Role of Information Technology in the Fight Against Tuberculosis

I have been working for 2 months now as a open source developer at TBCare project. Most of my work there consists of refactoring with occasional pattern designing and leadership. In short, most of the things you will find in a typical full-stack software engineering internship. However, I cannot help thinking that there is something missing in my line of work there. Working as a software engineer requires at least some degree of familiarity with your user. This has not been a problem when I worked for Dekoruma: I can somewhat imagine the needs of people working in interior design or simply wanting to buy a piece of furniture. But for TBCare, it is more tricky. I would be lying to myself if I say that I understand the plight of workers at the front line actively investigating and fighting the TB outbreak.
With that being the case at hand, it may be appropriate to look at the role of TBCare in the current attempt to eradicate TB. This article will look at the current problems with handling TB epidemic, what is being done, and how TBCare can be developed to further suit the needs of our brave doctors and investigators in the fight against TB.
We should start with knowing what Tuberculosis is. Tuberculosis is a bacterial infection mainly attacking the lungs that is spread through droplets from an infected person¹. It is caused by M. Tuberculosis. Symptoms of TB includes persistent cough, high temperature, night sweats, and fatigue.
For most healthy people, contact with M. Tuberculosis will be handled by the immune system. Normally, our immune system is capable of killing the bacteria and cause no symptoms. However, the bacteria can stay within a victim and remain dormant. This is known as latent TB. Should a person with weakened immunity become a latent TB host or get into contact with TB, that person will develop symptoms and become an active TB case. Left untreated, active TB case may become deadly.
Because TB is caused by bacteria, it can be treated with antibiotics. Unfortunately, the current set of drugs for TB requires 6 to 9 months of regular consumption to be effective². Failure to properly take medications will not only pose problems to oneself, but also create a drug resistance problem. Variants of TB known as Multi Drug Resistant TB (TB-MDR) has evolved³ and has been wrecking havoc on the current fight against TB.
So, that was the outline of what we need to know about TB: a contagious (Albeit less contagious than COVID 19) airborne disease caused by a bacteria called M. Tuberculosis. Considering how hard it is to treat this disease, it will be wise to just eradicate it. TB Eradication is one of United Nation’s Sustainable Development Goal, with reduction of TB cases by 90% is expected by 2030⁴. It is time to look on what should be done to fight TB.
Based on The End TB Strategy by World Health Organization, there are 4 challenges to the current TB eradication effort:
- Intervention funding Gap: An estimated US 1.4 billion per year of funding is yet to be available.
- Undetected cases: 3.6 million people are yet to be diagnosed and/or treated.
- Response to TB/HIV needs to be accelerated.
- TB-MDR cases also needs attention: Only one in four TB-MDR cases are detected and one in two cured.
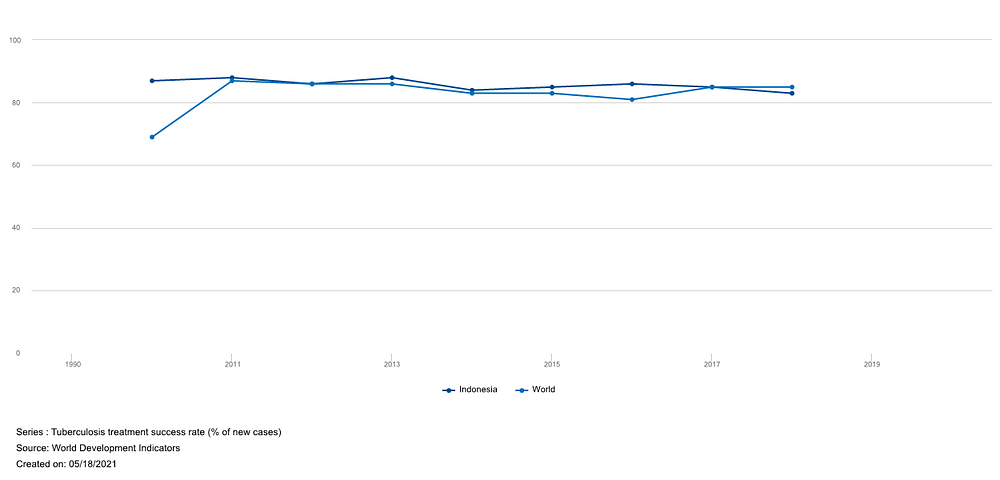
The above points are aggregated from the struggles worldwide and may not be representatives to the challenges in Indonesia specifically. However, it is a good starting point to look at how Indonesia fares globally in regards of TB eradication. Looking at Figure 1, it appears that point 2 is a more apparent problem in Indonesia compared to the rest of the world.

The percentage of successful treatment in Indonesia can also be an indicator that point 4 of End TB Strategy challenges has yet to be resolved in Indonesia. TB intervention success rate in Indonesia is steadily falling from 88% in 2011 to 83% in 2018. This trend may indicate an emergence of the harder-to-cure TB-MDR disease. Another possibility is the increase in recurring TB cases. Recurrent Tuberculosis is also harder to treat due to increased drug resistance, therefore reducing the chance of a successful treatment⁷.
Based on the two statistics above, we can conclude that the first step needed towards reducing active TB cases in Indonesia would be to increase case detection rate and reduce the number of recurrent TB cases. Ergo, the next objective is to find out the cause of TB recurrence. Systematic review in India⁸ conclude that irregular drug intake, initial drug resistance, smoking, and alcoholism are the main causes of relapse and recurrence. Another study from Tanzania⁹ conclude that the rural populations are at higher risk of recurrent case. Cases from remote areas have more limited access to medication individually, have a longer TB diagnosis delay, and seek treatment from traditional healers more frequently. Therefore, case detection and tracking at rural areas is important.
In conjunction with these related studies, WHO has also recognize that an “integrated, patient-centered TB care and prevention” is an important pillar in TB eradication⁴. An active-case findings initiative is crucial in order to close the case detection gap, prevent recurrent case from emerging, and reduce the probability of TB-MDR outbreak. This approach has been taken by PPTI, who have been sending out volunteers to investigate potential TB cases and keep track on medications of TB victims. So, one can argue that we are on the right path.
Let us look at what has been addressed in the current TBCare app and what hasn’t.
Current Progress
TBCare is made mainly for case monitoring. Both database and activity flow of the app is made with this in mind. For example, here is how a case is filed and monitored:
- Firstly, a reference case must be specified. Reference cases are active cases victim that may infect others. Note from before that TB is spread after long time contact with an active TB patient. This means that all cases can be tracked from their spreader.
- Secondly, patient’s relevant data are recorded, along with the history of screening and medication.
As we can see, the process above is similar with active case finding processes: After finding an active patient, quickly investigate every possible victim by looking at the patient’s physical contact history. This can be done more easily using the system above.
Another thing that the current TBCare app gets right is data management. Significant amount of development effort has been allocated in improving the way statistics are presented. The ability to filter cases based on districts is especially a good feature that has been added recently. Being able to see which area has been impacted the most will help in the prioritization of investigation effort.
Looking back at how TB prevention is done, the majority of design decision made from the very first sprint starts to make sense. It looks like the main problem for our doctors right now is data collection, and the current development path supports that.
What Can be Improved
It is good to see that TBCare is developing at the right path: Tracking as many cases with the least resource possible. And so, I think there is some other improvements that can be made. Firstly, the current data visualizations only classifies people as either positive cases or negative cases. There seems to be no record for MDR-TB. As stated by WHO, drug resistance is a major problem in TB eradication, and therefore should at least be recorded properly. By recording patients with MDR-TB, doctors can prioritize investigations around the said patients and prioritize follow-ups on patients with MDR-TB.
Secondly, data visualizations can be done better. One example of improvements is by providing a geographical heat-map of active cases. Because cases are spread through long term exposure, it is rational to think that areas near a TB hot spot is more likely to get infected than other areas. Providing this kind of visualization may improve prevention by putting nearby areas on higher alert.
Thirdly, patient should be allowed to participate in their recovery. Extending TBCare for patients will reduce the amount of follow-up needed for existing patients, especially in the urban area. An example of this is the Stay-Home Notice Tracking Solution by Singapore’s Ministry of Manpower. It allows people with stay-home notice to easily report their location regularly using GPS and photos. Perhaps the same can be implemented to monitor drug intake and allocate follow-up resources to other people without the necessary technology or in need of more supervision.
Lastly, it may be possible for TBCare to not just record individuals and areas with TB, but to create a prediction as well. The question “Given the record of TB cases in several areas, what is the likeliest area that will receive new TB case” might be answerable using regression models and machine learning. TBCare may not only become a web app, but also utilizes computers to create a prediction on where to prioritize investigations next, and how many volunteers are needed.
The main hindrance of the current active case finding initiative will be funding and resource allocation. Implementing extensive testing along with contact tracing like the policies enacted in Singapore during the COVID-19 pandemic is going to be costly¹⁰. Therefore, efforts must be made in order to lower the cost of tracking individual cases and/or increase the effectiveness of TB investigations. In both of these regards, the TBCare project has the potential to benefit the stakeholders in several ways:
- Becoming the main database of TB case reporting and tracking.
- Becoming a tool for investigators and analyst to point out areas that require interventions the most.
- Becoming an application that utilizes data science to automate contact tracing and predict the possibilities of an outbreak in certain areas.
As the world is starting to embrace the 4th Industrial Revolution, it is important for us to find the role of digital technology in the fight against TB. Lack of funding and resource is a real problem in our eradication effort. Therefore, the potential of computers to lessen the burden of tracking and predicting cases should not be overlooked, and may very well become the main tool for TB eradication in the future.
References:
[1] https://www.nhs.uk/conditions/tuberculosis-tb/
[2] https://www.cdc.gov/tb/topic/treatment/tbdisease.htm
[4] https://www.who.int/tb/End_TB_brochure.pdf
[5] https://data.worldbank.org/indicator/SH.TBS.DTEC.ZS
[6] https://data.worldbank.org/indicator/SH.TBS.CURE.ZS
[7] https://www.everydayhealth.com/tuberculosis/when-tuberculosis-infection-comes-back.aspx
[8] https://pubmed.ncbi.nlm.nih.gov/22628930/
[9] https://idpjournal.biomedcentral.com/articles/10.1186/s40249-018-0404-9
